Traditional skin grafts, often used for severe burns, involve transplanting a thin layer of epidermis from another part of the patient’s body. While life-saving, these grafts leave scars and fail to restore the dermis—the deeper skin layer containing blood vessels and nerves. Without a vascular network, grafted skin lacks the ability to fully integrate with the body, limiting its functionality. The Swedish team’s work addresses this challenge by creating artificial skin with integrated blood vessels, a critical step toward mimicking natural tissue.
Using a specialized bio-ink called “μInk,” researchers led by Jonas Junker have crafted a dense, cell-rich skin structure. Fibroblasts, cells that produce collagen and other dermal components, are cultured on tiny gelatin spheres and suspended in a hyaluronic acid gel. When printed in layers via a 3D printer, this bio-ink forms tissue that supports living cells. In mouse trials, the printed tissue not only survived but also integrated with the host, secreting collagen and fostering new blood vessel growth, indicating long-term viability.
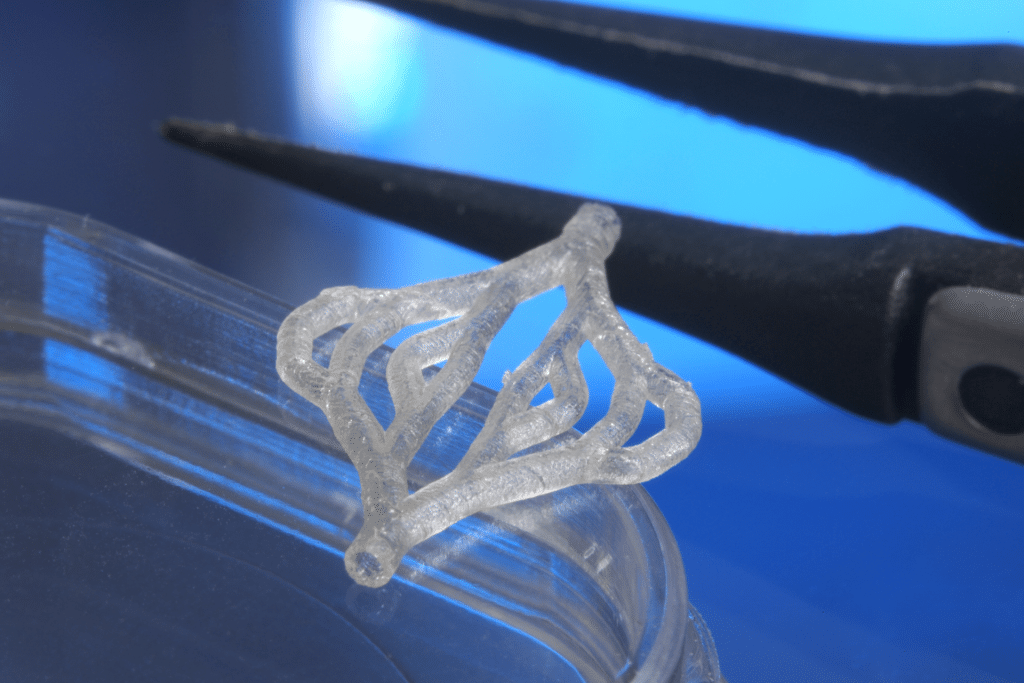
Innovative Micro-Tube Networks
The second technique, known as REFRESH (Real-time Extrusion-based Fabrication of Robust Engineered Systems for Hydrogel-based tissue engineering), focuses on creating intricate vascular networks. Researchers print a biodegradable hydrogel into threads, which are braided or knotted to form hollow micro-tubes resembling blood vessels. Once the hydrogel dissolves, these tubes allow fluid circulation, enabling blood vessel cells to grow within. This method, led by Daniel Aili, offers flexibility in designing complex 3D vascular structures, potentially applicable to entire organs.
The ability to pump fluids through these micro-tubes ensures that oxygen and nutrients reach all parts of the tissue, addressing a key barrier in regenerative medicine. By combining μInk and REFRESH, the team envisions creating thick, vascularized skin that can integrate seamlessly with a patient’s circulatory system, reducing the risk of rejection and improving healing.
Real-World Impact for Burn and Trauma Care
For patients with extensive burns or traumatic injuries, these advancements could be transformative. Current grafts often lead to scarring, reduced sensation, and limited functionality due to the absence of a dermis. The 3D-printed skin, with its vascular network, could restore more natural skin properties, such as elasticity and temperature regulation. In mouse experiments, the tissue showed promising integration, with new blood vessels forming within the graft, a critical factor for long-term success.
Beyond burns, this technology holds potential for treating chronic wounds, such as diabetic ulcers, where poor blood circulation hinders healing. By providing a vascularized framework, the printed skin could improve outcomes for patients who require frequent interventions, reducing healthcare costs and improving quality of life.
Challenges and Future Steps
Despite its promise, the technology faces hurdles before it can reach clinical practice. Inflammation and bacterial infections remain significant risks in wound environments, requiring rigorous testing to ensure safety. The Swedish team plans to automate the REFRESH process to create denser vascular networks, which could accelerate production and scalability. Further trials in larger animals and eventually humans will be necessary to validate these techniques.
The complexity of replicating skin’s full structure, including sweat glands and hair follicles, also poses a challenge. While the current focus is on vascularization, future iterations may incorporate these elements to enhance functionality and aesthetics. Collaboration with experts like Lars Kölby at Sahlgrenska University Hospital underscores the multidisciplinary effort needed to bridge lab results with real-world applications.
A New Era for Tissue Engineering
The development of 3D-printed vascularized skin marks a milestone in regenerative medicine. By addressing the critical need for blood circulation in artificial tissue, Linköping University’s innovations pave the way for more effective treatments for burns, trauma, and chronic wounds. As researchers refine these techniques, the dream of fully functional, lab-grown skin—and potentially other organs—moves closer to reality, promising a future where regenerative therapies redefine patient care.